August 13, 2024
As a reminder, providers in our commercial PPO network may see members of our new Coupe Health benefit plan starting in October 2024. This plan streamlines the payment process for your office and our Coupe Health members.
Coupe Health is a copay-only plan, and members pay no deductibles or coinsurance. You won’t collect any copay from Coupe Health plan members. Instead, Blue Cross and Blue Shield of Montana will reimburse you directly for the full allowed amount, including the member share.
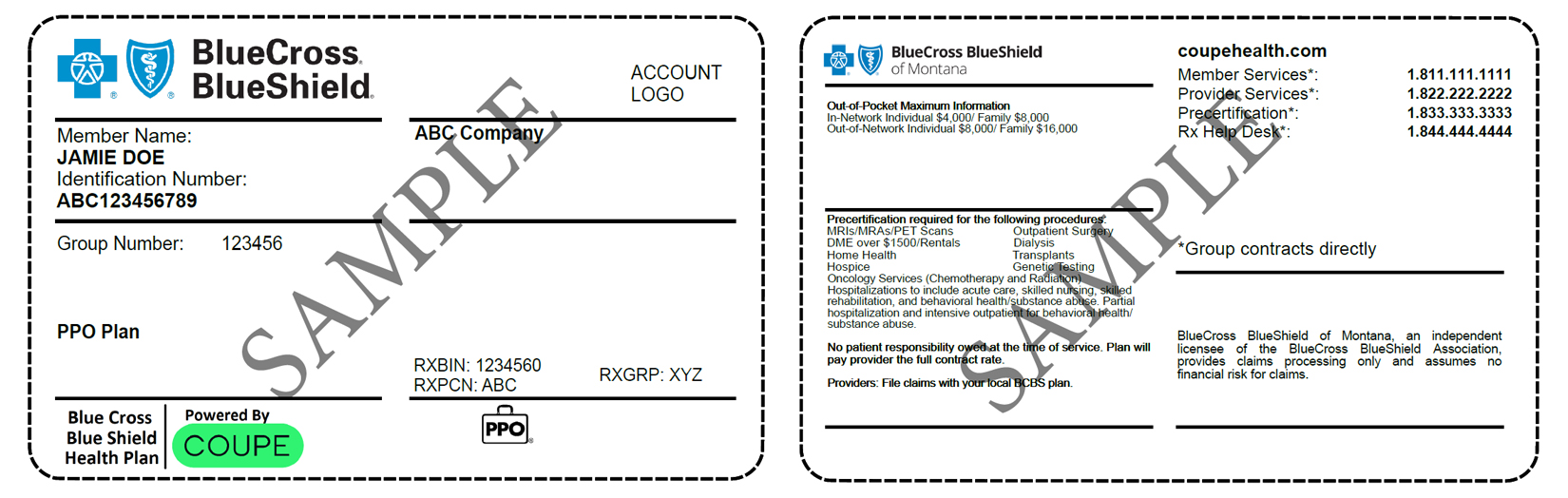
Look for Coupe on the ID card: As with all our members, it’s important to ask to see the member ID card before all appointments, and to check eligibility and benefits. Update your records if member ID numbers have changed. Use Availity® Essentials or a preferred vendor to check membership, coverage and prior authorization requirements, and to confirm that you are in-network for the member’s policy. Emergency services are covered at the in-network benefit level.
If you have questions, call the provider services number on the member ID card.
Availity is a trademark of Availity, LLC, a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSMT. BCBSMT makes no endorsement, representations or warranties regarding third party vendors and the products and services they offer.
Coupe Health is an independent company that has contracted with BCBSMT to provide an alternative health plan for members with coverage through BCBSMT.
Checking eligibility and benefits and/or obtaining prior authorization is not a guarantee of payment of benefits. Payment of benefits is subject to several factors, including, but not limited to, eligibility at the time of service, payment of premiums/contributions, amounts allowable for services, supporting medical documentation, and other terms, conditions, limitations, and exclusions set forth in the member’s policy certificate and/or benefits booklet and or summary plan description. Regardless of any prior authorization or benefit determination, the final decision regarding any treatment or service is between the patient and their health care provider.